On Dec. 3, 2020, the National Institutes of Health (NIH) announced updates to the clinical guidelines used to diagnose and manage asthma. The new guidelines are titled "The 2020 Focused Updates to the Asthma Management Guidelines: A Report from The National Asthma Education and Prevention Program Expert Panel Working Group." The National Heart, Lung, and Blood Institute (NHLBI), part of the NIH, oversaw the National Asthma Education and Prevention Program Coordinating Committee (NAEPPCC) and a 19-member expert panel working group that developed the guidelines. These are the first changes in 13 years to federal guidelines for children and adults with asthma.
Kenneth Mendez, the President and CEO of the Asthma and Allergy Foundation of America (AAFA), serves on the NAEPPCC and advocated for the voice of patients to be included in the guidelines. As part of our ongoing commitment to improving asthma health, AAFA is also supporting the rollout of the new recommendations to help make health information clear and accessible for the asthma community. AAFA is the only patient advocacy group on this committee.
The report includes 19 recommendations in six key areas of asthma diagnosis, management and treatment. Here is a general overview:
1. Using daily controller medicines as needed instead of daily
There are two types of asthma medicines: quick-relief and controller medicines. Quick-relief (“rescue”) medicines work fast to relieve or stop symptoms. Controller (“maintenance”) medicines are taken daily to prevent and control symptoms and asthma episodes. Controller medicines are also called inhaled corticosteroids (“steroids”), or ICS. Examples of ICS inhalers include QVAR® RediHaler™ (beclomethasone dipropionate), Flovent® (fluticasone propionate), ARNUITY® ELLIPTA® (fluticasone furoate), and ArmonAir™ Digihaler® (fluticasone propionate).
The updated guidelines include three options for taking ICS controller medicines. The first option is to take ICS every day to control asthma, and to use quick-relief medicine at the first sign of asthma symptoms. This recommendation is also in the previous guidelines.
A second and new option recommends that people with asthma take ICS controller medicines as needed. You will use your ICS and quick-relief medicine at the same time when you have symptoms. This can be as effective as using your controller medicine every day.
A third and also new option is a treatment option known as SMART (which stands for single maintenance and reliever therapy). SMART uses one inhaler that combines a controller and long-acting reliever medicine together. The inhaler contains an ICS and a medicine called formoterol [for-MOE-ter-ol]. Together, they act as both a daily control medicine and a relief medicine.
2. Using long-acting muscarinic antagonists (LAMAs)
Two types of asthma controller medicines keep the muscles around your airways from tightening and causing asthma symptoms: long-acting muscarinic antagonists (LAMAs) and long-acting bronchodilators (LABA). If your asthma is not well-controlled with ICS, the new guidelines recommend adding a LABA. If you cannot use a LABA, a LAMA may be a good option. If you are currently taking a LABA or LAMA medicine, don’t stop taking them without talking with your doctor.
3. Reducing indoor allergens (indoor allergen control)
The updated guidelines now offer steps you can take to reduce indoor asthma triggers. The report recommends that people with asthma take many steps (not just one!) to reduce or remove allergens. For example, using a mattress cover alone to reduce dust mites may not be enough. You may also need to vacuum often using a vacuum cleaner with a HEPA filter and wash bedding in hot water weekly.
In alignment with the new guidelines, AAFA’s CERTIFIED asthma & allergy friendly® program helps support a multi-component strategy to reduce certain asthma and allergy triggers found in homes and other indoor spaces. Our healthy home plan can also help you cut down asthma triggers in the home.
4. Allergy shots (immunotherapy as a treatment for allergic asthma)
Previous guidelines recommended allergy shots (immunotherapy) for people with allergic asthma. The updated guidelines also recommend allergy shots. The guidelines do not recommend sublingual immunotherapy (SLIT) – the tablet or drop placed under your tongue.
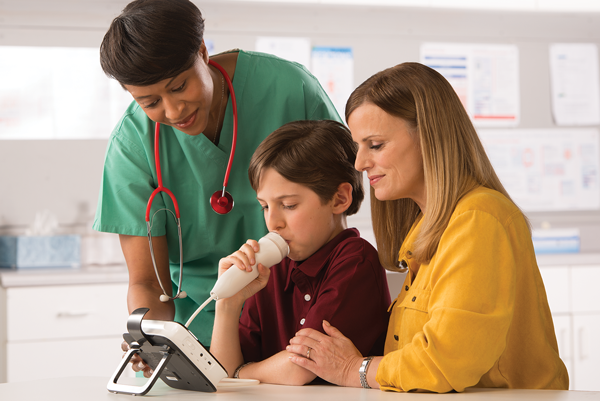
5. FeNO testing (fractional exhaled nitric oxide testing)
FeNO stands for fractional exhaled nitric oxide. Nitric oxide is a gas. If you have swelling in your airways, you will breathe out more nitric oxide. A FeNO test measures the amount of nitric oxide in your breath. This test helps doctors tell if and how much swelling you have in your airways. The updated guidelines recommend FeNO testing to diagnose asthma. Your doctor may use it with other lung function tests when asthma is difficult to diagnose.
6. Bronchial thermoplasty (BT)
Bronchial thermoplasty (BT) is a medical procedure. It is a series of three procedures that uses heat to remove smooth muscle tissue from the airways. This keeps muscles around the airways from tightening and causing asthma symptoms. This procedure is for adults with moderate-to-severe asthma. The updated guidelines do not recommend BT to treat asthma. Their findings show the benefits of the surgery are small. The risks are moderate, and long-term outcomes are uncertain.
Before making changes to your asthma treatment plan, talk with your doctor. This chart will help you know the differences between the previous guidelines and the new 2020 updates.
In the coming weeks and months, AAFA will be sharing more detailed information about the new guidelines.
People with asthma and their caregivers can also visit the NHLBI’s Learn More Breathe BetterSM program at www.nhlbi.nih.gov/BreatheBetter to learn more.
Kenneth Mendez, AAFA’s CEO and President invites you to join our community so you can receive more information about these guidelines and improve your asthma health:
“We’ll be working hard to make sure you have the information you need to feel confident when making health care decisions with your doctors.”
As a member of our community, you will:
- Get up-to-date information about asthma treatments
- Connect with other people living with asthma for support
- Have access to experts
- Be able to share your concerns so AAFA can advocate for you
- Become empowered to act on issues that impact people with asthma
- Be able to help advance research so we can save lives together



Comments (3)