Asthma is one of the most common chronic diseases in the U.S., affecting more than 27 million people. While up to 75% of people with asthma have mild disease, it can affect quality of life and may be deadly if it’s not well-controlled. The burden of asthma is greater for some communities. Black, Hispanic, American Indian, and Alaska Native populations have higher rates of asthma. Higher rates are seen in people in low-income communities as well.
Asthma During the COVID-19 Pandemic
The early lockdown period of the COVID-19 pandemic brought a surprising period of relief for many people with asthma. Asthma attacks declined. Some people reported easier breathing.
In May 2021, the Asthma and Allergy Foundation of America (AAFA) and Komodo Health published a research brief that further measured the impact of COVID-19 lockdowns. The project focused on race-based disparities in asthma-related emergency department visits. It compared emergency department rates in cities with high numbers of Black residents to cities with low numbers of Black residents.
The analysis found that while the total number of emergency department visits went down, race-based gaps grew. People living in cities with the highest number of Black residents were more likely to visit an emergency department with an asthma-related illness than people in cities with the lowest number of Black residents. The differences were stark.
For example, in New Orleans (60% Black population), about one in three residents with asthma visited the emergency department for a related condition at least once in 2020. This compares to only about one in 10 in Salt Lake City, where only 3% of the population is Black.
Asthma Since the Height of the COVID-19 Pandemic
Overall, asthma prevalence in the United States increased in 2022. More than 27 million people in the U.S. have asthma.
In a new analysis, we wanted to understand how race-based asthma disparities changed since the height of the COVID-19 pandemic. We looked at cities with the highest and lowest numbers of Black residents in 2022. Within these cities, we looked at severe asthma, emergency department visits, and prescriptions for quick-relief medicine.
Here’s what the new analysis found:
- People with asthma in cities with the highest number of Black residents were slightly more likely to have severe asthma compared to those in cities with the lowest number of Black residents.
In the six cities with the highest number of Black residents, 3.1% of people with asthma had severe asthma. This compares with 2.7% of people with asthma in cities with the lowest number of Black residents. - In 2022, roughly half of New Orleans residents with asthma visited the emergency department for an asthma-related illness.
People with asthma living in cities with the highest number of Black residents were 9% more likely to visit the emergency department in 2022 (40% vs. 31%). Of the cities included in this analysis, New Orleans (60% Black population) had the highest rate of emergency department visits. Half (49%) of the people with asthma in New Orleans visited the emergency department for a related illness in 2022. Portland (6% Black population) had the lowest rate at 25%.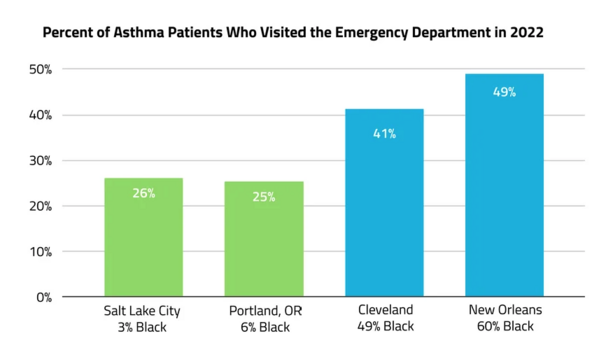
Differences in emergency department visits were much larger than those in asthma severity. This may be a result of social and structural determinants of health that can lead to an overreliance on emergency care. These include differences in insurance, care, and medicine access.
- The prescription rate for quick-relief drugs was 6% higher in cities with the highest numbers of Black residents. This includes both oral corticosteroids and non-steroidal medicines.
In 2022, 68% of people with asthma in cities with the highest number of Black residents had a prescription for a quick-relief drug. In cities with the lowest number, 62% of people with asthma received quick-relief prescriptions.
The difference in prescription rates was higher for steroidal drugs (7% higher) than non-steroidal drugs (5% higher). Oral corticosteroids (such as prednisone) may be prescribed to treat asthma attacks when a person hasn’t responded to other asthma medicines. Higher steroid medicine use may result from more severe or uncontrolled asthma.
Conclusion
Racial and ethnic disparities exist across most areas of health and health care. As in the case of asthma, socioeconomic and environmental inequities drive these disparities. The overall risk from these overlapping inequities makes asthma disparities greater.
The COVID-19 pandemic has highlighted the stark inequities that exist in the U.S. health care system. Health equity continues to be a focus now and will also be after the pandemic. Evidence based on data is key as we move to explain population-wide health disparities.
Data are also key to inform policy changes that address race- and ethnicity-based gaps in exposure, health, and care. This is particularly important for asthma. Disparities continue despite general improvement in asthma outcomes over the past 20 years. Population-based studies are critical to developing public health programs and improving asthma outcomes.
Methodology
This analysis looked at cities with the highest and lowest proportions of Black residents in 2022. We used ICD-10-CM codes to identify patients with:
- Severe asthma
- Asthma and one or more ED visits
- Asthma and a prescription for a quick-relief steroid medication
We then stratified the data by ZIP code using U.S. census data, grouping cities with a >40% Black population and a <10% Black population.
The cities with the highest proportions of Black residents were: Atlanta, Cleveland, Detroit, Memphis, New Orleans, and Washington, D.C.
The cities with the lowest proportions of Black residents were: Austin, Phoenix, Portland, Salt Lake City, San Diego, and Seattle.
About Komodo Health
Komodo Health is a technology platform company creating the new standard for real-world data and analytics. Komodo pairs the industry’s most complete view of patient encounters with enterprise software and machine learning to connect the dots between individual patient journeys and large-scale health outcomes. Across Life Sciences, payers, providers, and developers, Komodo helps its customers unearth patient-centric insights at scale. The company marries clinical data with advanced algorithms and AI-powered software solutions to inform decision-making, close gaps in care, address disease burden, and help enterprises create a more cost-effective, equitable, and value-driven healthcare system. For more information, visit komodohealth.com.
This content was adapted from content published by AAFA and Komodo. Race-Based Disparities in Asthma: A Post-Pandemic Snapshot © 2023 Komodo Health, Inc. All rights reserved. Reproduction, distribution, transmission or publication is prohibited. Reprinted with permission.
AAFA thanks Amgen and PCMA Foundation for 2022-2023 research funding that helps AAFA access data from Komodo Health.

Comments (0)