Black Americans bear a much higher burden of asthma than white Americans. Compared to white Americans, Black Americans are five times as likely to visit the emergency department due to asthma, two times as likely to stay in the hospital due to asthma, and three times as likely to die from asthma. This is why reducing asthma disparities is a critical part of the mission of the Asthma and Allergy Foundation of America (AAFA).
Despite these statistics, people like Linda Nozart are making an impact within their local communities. In honor of Black History Month, AAFA spoke with Linda about the important work she does.
About Linda Nozart, MPH, BSRT, RRT, AE-C
 Linda Nozart is the Administrative Director of the Asthma Program at NYC H + H/Woodhull Hospital (part of the NYC Health + Hospitals health system). She oversees the NYC Department of Health Asthma Center of Excellence CHW Asthma Case Management Program. The program works to reduce emergency room (ER) visits for children with asthma.
Linda Nozart is the Administrative Director of the Asthma Program at NYC H + H/Woodhull Hospital (part of the NYC Health + Hospitals health system). She oversees the NYC Department of Health Asthma Center of Excellence CHW Asthma Case Management Program. The program works to reduce emergency room (ER) visits for children with asthma.
For more than 13 years, she has led asthma steering committees, interdisciplinary workgroups, and allied coalitions as a registered respiratory therapist (RRT) and certified asthma educator (AE-C). She served four years as the Chairperson of the North Brooklyn Asthma Action Alliance (NBAAA), an award-winning asthma coalition that caters to reducing disparities in health care by serving medically underserved communities and providing access to quality care.
Linda Nozart received her Bachelor of Science in Respiratory Care and Master of Public Health at Long Island University Brooklyn (LIU). She is currently the CEO of Noz Health ED, LLC (a health care consultant business), the host of the "RTs Share Tea" podcast, and a public speaker on asthma education and community health program development.
Q: What led you to work with people with asthma?
Linda: I've had asthma since the age of 8 years old. I'm the first American born to my Haitian immigrant parents. They knew very little about the disease. As a young child who spoke English, I had to help my parents navigate through the health care system. At that point I was at my sickest, having asthma attacks mainly at night. My parents were afraid I was going to die in my sleep, so I had to share the bed with my parents for a year.
I also know how it is to feel like a burden to the family as a sick child being the only one in my family to have asthma. I watched my parents choose between paying my medical bills and for my medication or paying the utility bills. There were nights when my siblings and I had to do homework next to candles and go to sleep with coats. I started working at the age of 14 to help my family with these financial burdens. As a result, I knew I would always work in the health care field in some shape or form to help others.
Q: Why you are passionate about working to end asthma disparities?
Linda: I truly understand how uncontrolled asthma can seriously affect quality of life for families. My interest in asthma management really grew in 2010 when I was covering a pediatric ER as a registered respiratory therapist.
During my night shift at a level 1 trauma center, I had placed a 5-year-old African-American boy on a ventilator after he went into cardiac arrest three times due to a severe asthma attack.
I had a strong feeling he was not going to make it that night and he didn't. It was the first time I cried after my shift. When my husband asked me why I was crying – because he knew I had seen children pass away before – I said strangely it was not for the boy, but for his family. The child had his asthma attack while an extended family member was watching him. They didn’t know how to recognize the signs and symptoms of an asthma attack. That broke my heart. I never wanted to see this happen to another family.
As a result, I got certified as an asthma educator the same year, which sent me on the path to get my Master of Public Health with a focus on health promotion and education to fully understand why these things happen in certain communities. With everything I have personally experienced and seen both in and out of my career around asthma, my intentions – no matter the communication vehicle – are always to spread asthma awareness and access to resources to fight asthma disparities.
Q: What is your favorite part of the work you do with the asthma community?
Linda: When I first got the position and realized I had community health workers (CHWs) on my team, the first thing I had to do was research what a CHW truly was and their scope of practice. It was a little challenging to lead a team that had members that did not come from a clinical background.
As an RT, I had to scale back and put my public health hat on to empower the team to advocate for the community we serve. The CHWs reflected the community and wanted to help those with uncontrolled asthma improve their quality of life. That meant everything to me as a person that has a passion for asthma self-management education. So, I invested the time in designing asthma education material so that our CHWs would be able to guide a patient successfully along the journey toward asthma control.
I love what our pediatric CHW asthma case management program has become. The community trusts us, and we get to see real progress by providing home assessments, linkage to specialty practice, and social services keeping them from unnecessarily having to return to the ER for asthma. As a result of successfully integrating CHWs into the interdisciplinary team, I was one of the lead trainers for the hospital’s home-based asthma program.
Q: Is there anything else you’d like to share as you reflect upon Black History Month and your work?
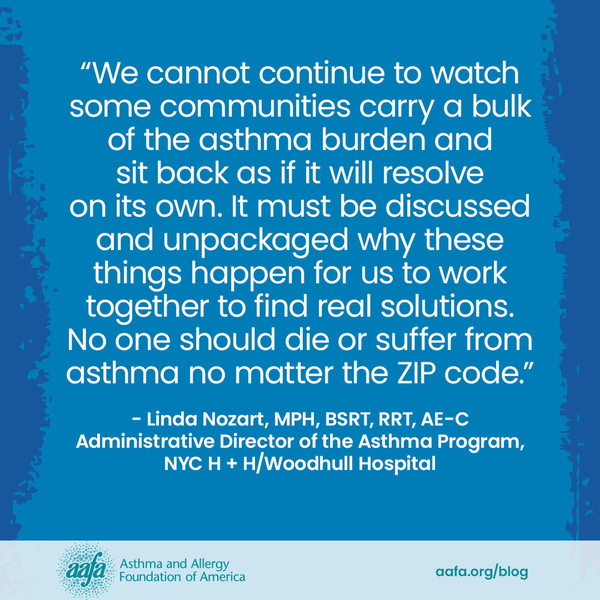
Linda: We cannot continue to watch some communities carry a bulk of the asthma burden and sit back as if it will resolve on its own. It must be discussed and unpackaged why these things happen for us to work together to find real solutions. No one should die or suffer from asthma no matter the ZIP code.
“Selling” health is not easy. You need patience, empathy, and passion to carry you. Most patients with uncontrolled asthma in minority communities have "onion layers" of social and economic barriers toward health. You genuinely have to understand someone's journey to guide them toward asthma control. Seeing someone's quality of life improve because of your work is very rewarding. I love what I do. That’s why everyone calls me “Thee Asthma Lady.”
How Can You Help Reduce Asthma and Allergy Disparities?
The only way we can reduce health disparities is if we all work together. Everyone – from people with asthma and allergies to policymakers and the health care industry – can be a part of building programs that make a lasting difference for people, families, and communities impacted by asthma and allergies.
Sign up for AAFA’s community to stay up to date about the following opportunities to get involved:
- Advocate for people affected by asthma disparities
- Participate in patient-centered research and clinical trials
You can also donate to support AAFA’s mission to create real and lasting change.


Comments (0)