A Personal Story from the Asthma Capitals™ 2018 Report
On May 1, 2018, – World Asthma Day – the Asthma and Allergy Foundation of America (AAFA) released the Asthma Capitals™ 2018 report. This report ranks the top 100 Asthma Capitals in the U.S. It highlights the widespread impact asthma has on our nation. For 25 million Americans, asthma is a challenging disease that can have physical, emotional, social and financial impacts. During National Asthma and Allergy Awareness Month, we will share personal stories from our top 20 capitals to show what life is like managing asthma.
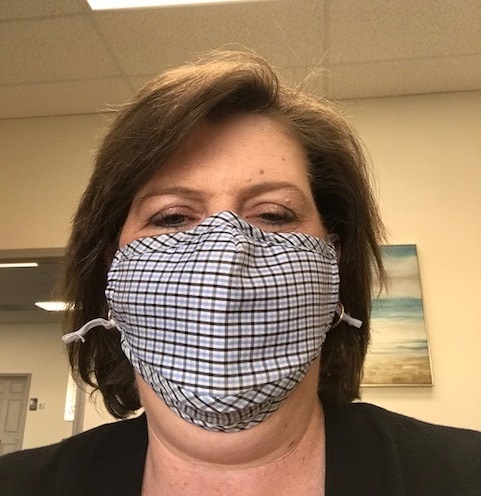
Lynn Johnson
#8 Asthma Capital: Birmingham, Alabama
For many, asthma is caused by an allergic reaction to something. This is called allergic asthma is the most common. But a small number of people with asthma have “non-allergic asthma.” Lynn Johnson is part of this group.
Lynn developed non-allergic asthma seven years ago, as an adult. It took quite some time to pinpoint what her triggers are. Lynn keeps a daily journal of her symptoms, the weather and what’s going on in her life. After analyzing three years of this data, she was able to identify a few patterns. Lynn found that her asthma is often triggered by weather changes, cold air, strong smells and stress. Sometimes, though, the trigger for a particular asthma attack remains a mystery.
Lifestyle Changes
A big challenge for Lynn has been the lifestyle changes that her asthma required. For example, to avoid strong smells Lynn switched to using only scent-free products.
“Literally anything that comes into my house must be scent-free,” she says. This includes cleaning products, deodorant, soaps, shampoo and more. This goes for the products that Lynn’s husband and two teenage sons use, too. Even her sons’ friends know not to wear any perfumes, colognes or other scented products when they come over to the Johnson’s house.
Lynn’s problems with scents makes her afraid to go into other people’s homes.
“They may have plug-in air fresheners, perfume, smoke, potpourri,” Lynn points out. “All of those at any given time will give me a problem. Once I have a problem, it tends to go downhill really fast and can take weeks to recover.”
While Lynn has a few friends who go the extra mile to make their homes safe for her to visit, when they socialize, the Johnsons usually choose to be the hosts.
Exercise has always been important to Lynn. She walks, jogs, rides stationary bikes and until three years ago was active in martial arts. Now there are times when she can exercise every day, and other times when she may have to go a month or two without being able to do much exercise at all.
“Even if I only have enough breath to walk a half a mile,” Lynn states, “I try to get something in. Anything is better than nothing!”
While these things are significant, Lynn’s biggest change has been at work. Once she understood that stress plays a major role in her asthma, she completely changed her job and career.
“I was hospitalized three times in less than a year,” Lynn shares. “Then the fourth time I spent three days in the Medical Intensive Care Unit (MICU), and then took 30 days of medical leave from my job to recuperate. This was a ‘slap in the face’ for me that the way I was managing my asthma would kill me. I was working 55 to 60 hours a week in a high-stress job. I had to get out of the stress! Now, in my new career, I have set hours and much less stress.”
Lynn has not been hospitalized again since she made the switch.
Getting Comfortable With the Nebulizer
From the medical standpoint, non-allergic asthma cannot be helped with allergy treatments. After all, it’s not caused by allergies. Medicine and trigger avoidance are the main treatment options. This means that keeping up with her medicines is very important for Lynn. In addition to her maintenance medicines, sometimes Lynn needs her quick-relief medicine every two to three hours around the clock. Other times she can go several weeks without it.
To make things even more challenging, though, Lynn cannot use inhalers.
“There’s something in the propellant that my lungs don’t like,” she states. “So every bit of medication I take must be via nebulizer. I have a hand-held nebulizer that I carry. It goes with me everywhere. And I have a regular portable nebulizer in the car, one in my desk at work and a few at home. Even when I’m walking I’ll have a cell phone and a nebulizer in my hand. I don’t go anywhere without it. It’s my rescue medication.”
Lynn also keeps a carbon filter mask in her purse. She’ll use it if she cannot avoid strong scents, such as someone’s perfume, and during flu season.
Lynn has been very self-conscious about these things. She feels it’s embarrassing to have to use a nebulizer out in public. But AAFA’s online asthma support group has helped Lynn get past this.
“Through their support and encouragement I’m not as self-conscious to use nebulizers when I need to,” she acknowledges. “And I’m also not self-conscious about wearing a mask when I’m not in my house.”
Family Support
For Lynn, asthma is a year-round challenge. Luckily, her family has been very supportive and accommodating.
“They can tell if I’m having trouble,” Lynn relates, “and they kick in to help and take care of things around the house. They do what they can to include me in their daily lives if I can’t participate. And they understand that sometimes I just don’t have the air to carry on a conversation with them. But I can listen.”
Her family is also supportive of some of the changes they have had to make at home. For example, they must have a generator for the nebulizers. Vacations, outings and socializing all require a lot more planning and awareness. Lynn’s asthma affects the family’s budget, too.
“The medicine applies to my deductible. My two maintenance meds alone are over $2,000 a month,” Lynn shares. “Thankfully my primary care doctor is willing to get samples of at least one of those for me, and that helps tremendously. Without that I couldn’t put out that kind of money each month. The nebulizers are expensive, and the insurance will not pay for my portable ones. Plus, we live in an area with poor air quality, and the in-cabin air filter in our cars must be changed regularly. Those are $80 each.”
Managing Asthma in Birmingham
One of the issues facing those with asthma who live in the Birmingham area is poor air quality.
Birmingham also has an extreme shortage of pulmonologists who will treat asthma patients. In her area, Lynn says that for people who have severe asthma, the allergists only want to manage the associated allergies. They refer patients to pulmonologists for management of the asthma. But most of the pulmonologists in the area want to focus on treating people with sleep disorders. For those that will treat asthma patients, there is a very long wait.
“In the last one-and-a-half years I called every pulmonologist office in town,” Lynn states. “The shortest amount of time to get in was 11 months. I was told that if I had a problem in the meantime, I should go to the emergency room.”
Lynn’s Advice to Others With Asthma
“More than anything, you have to be an advocate for yourself,” Lynn observes. “You have to find a physician who you’re comfortable working with and talking to. Because it’s a whole lot of trial and error and not many people understand. If you’re not comfortable talking to your doctor about what’s going on with you, there’s always the chance that you’re not getting your asthma as controlled as you could.”
“Also,” Lynn adds, “even though lifestyle changes have to be made, it doesn’t mean your life stops. You learn to work around it. Stay as active as you can. Enjoy life. You have to make accommodations for it, but asthma doesn’t have to run your life.”
JOIN NOW
The Asthma Capitals™ 2018 report is an independent research and education project of the Asthma and Allergy Foundation of America made possible with support from Sanofi Genzyme and Regeneron.


Comments (2)