With the current spread of the new coronavirus (COVID-19) in the U.S. and around the world, many people with asthma wonder how it would affect them if they got the illness. There is a lot we still don't know about this illness. Dr. Mitchell Grayson, the chair of the Asthma and Allergy Foundation of America's (AAFA) Medical Scientific Council, wrote this article for our blog about what we do know at this time.
There have been many questions about how having asthma affects your risk of getting the new coronavirus (COVID-19), as well as how severe the infection will be, if you do get infected. Let me explain a little about the current situation on available published data on asthma and COVID-19 (as of the morning of March 12, 2020). At this time, there is very little clear data to demonstrate a specific increased risk for COVID-19 from asthma. The CDC still lists asthma as a comorbid condition that can increase your risk, but there are scant published data to support this contention. The published data comes from China, where asthma was NOT noted to be a risk factor in studies.
However, it is important to note that asthma appears to be under-diagnosed and reported in China.1 One study of 140 patients found none with asthma2, and in a larger study of 1099 patients, asthma was not noted.3 In this larger study, chronic obstructive lung disease (COPD) was noted in patients hospitalized with COVID-19, but the rate of patients with COPD who had COVID-19 (1.1%) was lower than the rate of COPD in the general Chinese population (at least 10%).4 Together these data would suggest the risk of COVID-19 is actually lower in those with asthma or COPD; however, these data are based on hospitalized patients, so we don’t really know the overall risk. Also, as I have mentioned before, other coronaviruses have been shown to exacerbate asthma, so it is possible that COVID-19 will do so, as well. In particular, asthma has been shown to be a risk for MERS (Middle Eastern Respiratory Syndrome) coronavirus (MERS-CoV) infection (31% of those with MERS in one study had asthma).5 It is possible, that because of this association with MERS (and an association of regular circulating coronaviruses with asthma exacerbations) that asthma became listed as a potential risk factor for severe COVID-19.
So, the upshot is that the data are limited and at this time do not demonstrate any clear evidence of increased risk of disease or severity of disease for those with asthma. However, it is important that all patients with asthma take their medications and keep their asthma under control. Avoid people who have recently (within 14 days) traveled to China, Italy, South Korea, Japan and Iran (and any other country that has a CDC Level 2 or 3 warning), or who have been or are sick. If you live in a region with community spread of COVID-19, please practice social distancing (stay 6 or more feet away from individuals who appear ill, are coughing, etc., and avoid all large crowds). Remember to wash your hands frequently and to wipe down any surfaces you are going to touch in public areas with a disinfectant wipe. If you feel ill (and especially if you have a fever), please stay home and call your medical provider for additional advice.
One final issue about the data that say corticosteroids are possibly dangerous in COVID-19. These data come from hospitalized patients where the use of systemic corticosteroids after onset of the disease as a treatment for COVID-19 demonstrated a poorer outcome. There are no data available on a risk for those taking corticosteroids (orally or inhaled) for their asthma and a risk of poor outcome from COVID-19. So, as of now there is no reason to stop taking your controller medications. Let me say that again:
Please DO NOT STOP TAKING YOUR ASTHMA MEDICATIONS without talking with your health care provider!
This is a scary time for all of us, but we will get through this. Please continue to follow AAFA's blog on COVID-19 and asthma for more updates as data become available.
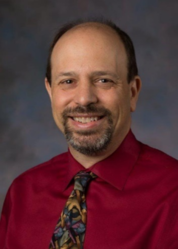 Mitchell Grayson, M.D., is a professor of pediatrics and chief of the Division of Allergy and Immunology at Nationwide Children’s Hospital and The Ohio State University. He is the Grant Morrow, III, MD Endowed Chair in Pediatric Research.
Mitchell Grayson, M.D., is a professor of pediatrics and chief of the Division of Allergy and Immunology at Nationwide Children’s Hospital and The Ohio State University. He is the Grant Morrow, III, MD Endowed Chair in Pediatric Research.Dr. Grayson’s clinical interests are primarily asthma, allergic rhinitis, food allergy and anaphylaxis. He oversees an active laboratory funded by the National Institutes of Health (NIH) studying the role viral infections play in the development of allergic disease.
Dr. Grayson received his medical degree from the University of Chicago, Pritzker School of Medicine. After completing an internal medicine residency at the Hospital of the University of Pennsylvania, he undertook his allergy/immunology fellowship at Johns Hopkins University.
Dr. Grayson is a board-certified diplomate of the American Board of Allergy and Immunology and an active fellow of the AAAAI and ACAAI. He is a director for the American Board of Allergy and Immunology and is on the board of directors of the Asthma and Allergy Foundation of America, as well a member of the Scientific Advisory Committee of the American Lung Association. Dr. Grayson has served on numerous grant review study sections for the NIH and has been on several editorial boards for allergy and immunology journals.
References
1. Huang, K., Yang, T., Xu, J., Yang, L., Zhao, J., Zhang, X., … China Pulmonary Health (CPH) Study Group. (2019, August 3). Prevalence, risk factors, and management of asthma in China: a national cross-sectional study. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/312308282. Zhang, J.-J., Dong, X., Cao, Y.-Y., Yuan, Y.-D., Yang, Y.-B., Yan, Y.-Q., … Gao, Y.-D. (2020). Clinical characteristics of 140 patients infected with SARS‐CoV‐2 in Wuhan, China. Allergy. doi: 10.1111/all.14238
3. Guan, W.-J., Ni, Z.-Y., Hu, Y., Liang, W.-H., Ou, C.-Q., He, J.-X., … Zhong, N.-S. (2020). Clinical Characteristics of Coronavirus Disease 2019 in China. New England Journal of Medicine. doi: 10.1056/nejmoa2002032
4. Wang, C., Xu, J., Yang, L., Xu, Y., Zhang, X., Bai, C., … China Pulmonary Health Study Group. (2018, April 28). Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/29650248/5. Kerkhove, M. D. V., Alaswad, S., Assiri, A., Perera, R. A., Peiris, M., Bushra, H. E. E., & Binsaeed, A. A. (2019). Transmissibility of MERS-CoV Infection in Closed Setting, Riyadh, Saudi Arabia, 2015. ;Emerging Infectious Diseases, 25(10), 1802–1809. doi: 10.3201/eid2510.190130

Comments (8)