Asthma affects 5.1 million American children.1 It is one of the most common serious chronic disease in kids. The burden of asthma is even higher among Black, Hispanic, and American Indian/Alaskan Native children. Because children may not always understand asthma and its symptoms, parents face a variety of challenges as they try to help their children breathe.
Emily Nkele knows just how challenging childhood asthma can be. Her son, Karabo, has had severe asthma for most of his young life. He is like many 5-year-olds – active and outgoing with an intense love for LEGO. But managing his asthma has kept his parents on their toes.
View this post on Instagram
What Asthma Looks Like in Children
In children, asthma can look a little different than it can in adults. In infants and toddlers, asthma is often triggered by viral infections. It can be hard to diagnose because it can look like other childhood illnesses, such as respiratory infections. Sometimes, asthma doesn’t really show signs in infants and toddlers until they get sick with a respiratory infection. That’s exactly what happened to Karabo.
“When he was born, his respiratory rate was super fast, so [the doctors] were always wondering what was going on,” Emily recalled. “They were questioning if he had some sort of lung disease. Then when he was 5 months old, he got RSV. And he was in the ICU – he was on a breathing tube in an ICU for 12 days. After that, for about six months, he was doing better. But he wasn’t quite fully recovered. He just still had a hard time breathing. All the breathing symptoms that go with respiratory viruses were still there. So we took him to the doctor, and at about a year old she said, ‘I think we need to consider this as more than just recovering from RSV and that there’s an underlying problem here.’”
In children ages 7 to 11, asthma is most often triggered by allergens and exercise. Cold weather, tobacco smoke, and seasonal allergies are most likely to trigger severe asthma attacks.2
In puberty, girls are at a greater risk for asthma than boys. Hormones may have some effect on changes in asthma. Children 12 to 17 see the greatest impact on school attendance and their ability to play sports and sleep.2 Asthma is the top reason for missed school days.3
Common Asthma Signs and Symptoms in Infants and Younger Children
- Fast breathing
- Panting with normal activities such as playing
- Wheezing (a whistling, squeaky sound when you breathe)
- Persistent coughing
- Difficulty sucking or eating
- Tiredness, not interested in normal or favorite activities
- Nostrils flaring
Severe Asthma Signs and Symptoms in Infants and Younger Children
Call your child’s doctor or 911 right away if your child has the symptoms below!
- Working harder to breathe (with nostrils flaring, skin is sucking in around and between ribs or above the sternum, or exaggerated belly movement)
- Tissue color changes on mucus membranes (like lips and around the eyes) and fingertips or nail beds – the color appears grayish or whitish on darker skin tones and bluish on lighter skin tones
These are some more common signs and symptoms and may change based on age and physical development.
Managing and Treating Asthma in Children
Sometimes children with asthma – especially young children – have trouble recognizing symptoms or saying what’s happening when they are having asthma symptoms. They can easily become preoccupied while playing and not notice when something is wrong. They may seem normal until symptoms suddenly get worse. This means parents, caregivers, and teachers have to watch children with asthma carefully to notice and treat symptoms before they become severe.
“Karabo fools a lot of people because he always looks happy,” said Emily. “He usually has energy. But that’s not always the case. He likes to not tell us because he has a fear of missing out on things. So he will wait to tell us until it’s extremely bad. And I also think because as long as he can remember he’s had a hard time breathing, he doesn’t really know how to tell us his asthma is getting worse. Because at that point, he was used to never being able to breathe, and so it didn’t seem extreme to him.”
View this post on Instagram
An asthma management plan is the same for both adults and children. The goal of the management plan is to prevent asthma episodes and help your child keep their asthma under control. A treatment plan includes:
- Learning your child’s triggers and help avoid them
- Giving allergy and asthma medicines as directed by the doctor
- Tracking their asthma and recognizing early signs that it may be getting worse
- Knowing what to do when asthma is getting worse by having an Asthma Action Plan
Children can also safely take many of the same asthma medicines as adults, if they are taken correctly. These may include a controller medicine they take regularly to prevent asthma symptoms from happening and a quick-relief medicine they take to relieve sudden symptoms. Or your child’s doctor may prescribe a combination medicine that can provide both short-term relief and long-term control based on the newest clinical guidelines. To learn more about this method of treatment, talk with your child’s doctor.
Some studies show the use of daily controller medicines may slightly affect a child’s growth. But asthma is a much greater risk to their health and quality of life.
Infants and younger children may use a device called a nebulizer to take their asthma medicines. A nebulizer machine, or “breathing machine,” turns liquid asthma medicine into a mist. Your child then breathes in the medicine through a mask or mouthpiece. A doctor can prescribe a nebulizer and the liquid medicine that goes into the nebulizer. They can come in tabletop models, as well as portable models you can take with you. Emily and Karabo prefer to use a nebulizer for his quick-relief treatments.
Inhalers with spacers or valved holding chambers work well for many children, too. These devices attach to metered dose inhalers (MDI) and help the medicine get into the lungs. Infants and young children can use a spacer or valved holding chamber with a mask that covers their mouth and nose.
Talk with your child’s doctor about what device will work best for them.
View this post on Instagram
Tips for Managing Your Child’s Asthma
It is possible to successfully manage your child’s asthma. Here are some things to remember:
Work with your child’s doctor to create an Asthma Action Plan. An Asthma Action Plan has information and instructions on how you can manage your child’s asthma. It includes medicine instructions, what to do when symptoms get worse, and what to do in an emergency.
Learn your child’s asthma triggers. Your child’s doctor can help you figure out their triggers. Then you can work to reduce triggers at home. AAFA has created a Healthier Home Checklist to help you improve your home environment. Contact your child’s school nurse to discuss asthma triggers at school.
Learn to recognize your child’s symptoms and early warning signs. Younger children may not always understand when they are having symptoms, or they may not want to stop what they are doing to tell you. Older children may be too embarrassed to say anything or want to avoid attention. Early warning signs in children can include moodiness or feeling tired.
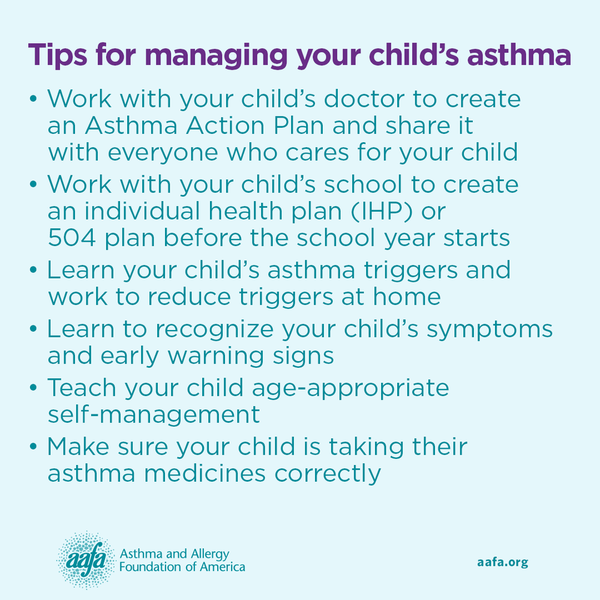
Share your child’s Asthma Action Plan with everyone who cares for your child. This includes friends, family, babysitters, teachers, school nurses, and coaches.
Work with your child’s school to create an individual health plan (IHP) or 504 plan before the school year starts. Include an updated version of your child’s Asthma Action Plan. Work with teachers and caregivers to help them understand signs, treatment, and importance of reducing trigger exposure.
Teach your child age-appropriate self-management as they grow. As your child gets older, they will have to be able to know how to manage their asthma on their own. For example, start by teaching your child to tell an adult when they have symptoms. As they get older and learn to read, you can teach them how to read their Asthma Action Plan. And teach them to always carry their quick-relief medicine with them at all times in case sudden symptoms appear. Students in all 50 states have the right to self-carry their emergency asthma medicines at school. Just be sure you have filled out the required school paperwork.
Make sure your child is taking their asthma medicines correctly and as prescribed. Talk with your child’s doctor about which medicines and devices will work best for your child. If your doctor recommends a nebulizer, you may need to order the nebulizer, tubing, and medicine cups from a durable medical equipment (DME) company or your local pharmacy. Work with your doctor and insurance company to find a nebulizer model that is covered by insurance and will work best for you.
Avoid buying devices labeled as “vaporizers” on online sites, like Amazon. They may not properly deliver the medicine to your child’s airways. Also avoid essential oils, even ones that claim to help with breathing. They can irritate your child’s airways and cause asthma symptoms.
Medical Review June 2021 by S. Allan Bock, MD, and Maureen George, PhD, RN, AEC, FAAN
References
1. Centers for Disease Control and Prevention. (2020). 2019 National Health Interview Survey data. U.S. Department of Health & Human Services. Retrieved from: https://www.cdc.gov/asthma/nhis/2019/data.htm
2. Trivedi, M., & Denton, E. (2019). Asthma in Children and Adults-What Are the Differences and What Can They Tell us About Asthma?. Frontiers in pediatrics, 7, 256. https://doi.org/10.3389/fped.2019.00256
3. Centers for Disease Control and Prevention. (2015). Asthma-related missed school days among children aged 5-17 years. U.S. Department of Health and Human Services. https://www.cdc.gov/asthma/ast...ats/missing_days.htm





Comments (0)