We have updated this blog post to reflect the most recent recommendations from the Asthma and Allergy Foundation of America (AAFA) and the Centers for Disease Control and Prevention (CDC).
As more information becomes available, we will continue to update our community.
The COVID-19 vaccine is an important part of reducing the spread of the coronavirus, ending the pandemic, and protecting ourselves and other people. It can reduce your chance of severe COVID-19, hospital stays, and death.
What Do I Need to Know About the COVID-19 Vaccines Currently Available?
The COVID-19 vaccine is safe and easily available throughout the United States for anyone 6 months and older. There are currently four vaccines: Pfizer, Moderna, Johnson & Johnson (J&J), and Novavax. The Centers for Disease Control and Prevention (CDC) recommends that people ages 5 and older get booster shots after completing the primary series, or first dose(s). Information on each vaccine, their recommended schedules, and boosters are detailed in the article below.
Pfizer COVID-19 Vaccine, Also Known as COMIRNATY®, for Everyone 6 Months and Older
COMIRNATY® [koe-MIR-nah-tee] by Pfizer is an mRNA vaccine. It is one of the mRNA vaccines recommended for anyone ages 6 months and older. The CDC’s recommended vaccine schedule is below.
If you or your child are moderately-to-severely immunocompromised, you will have a different vaccine schedule. This includes children and adults on high doses of corticosteroids (like prednisone), who have received an organ transplant, or have other serious health conditions.
Children 6 months to age 4
- Primary doses: Three doses three to eight weeks apart
- Booster doses: Not recommended at this time
- Immunocompromised:
- Three primary doses (first two doses three weeks apart and the third at least eight weeks after the second dose)
- Three primary doses (first two doses three weeks apart and the third at least eight weeks after the second dose)
People ages 5 to 11
- Primary doses: Two doses three to eight weeks apart
- Booster dose: At least five months after the second dose
- Immunocompromised:
- Three primary doses (first two doses three weeks apart and the third at least four weeks after the second dose)
- One booster (at least three months after the third primary dose)
People ages 12 and older
- Primary doses: Two doses three to eight weeks apart
- Booster dose: At least five months after the second dose
- Immunocompromised:
- Three primary doses (first two doses three weeks apart and the third at least four weeks after the second dose)
- Two boosters (the first one at least three months after the third primary dose and the second one at least four months after the first booster)
People ages 50 and older should get a second mRNA booster at least four months after the first booster.
If you got the Pfizer vaccine for your first shot, the CDC recommends that you get the Pfizer shot for your additional primary shots.
Children 5 to 11 years of age will receive a lower dose of the vaccine than people 12 and older. If you have any questions about the vaccine for your child, talk with your family doctor or pediatrician.
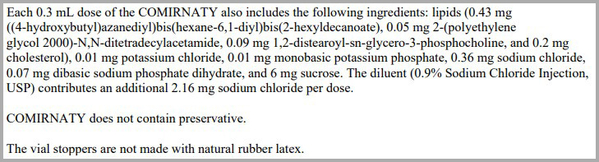
Pfizer COVID-19 Vaccine Ingredients
The Pfizer vaccine does not contain any food proteins, latex, or preservatives. It does contain mRNA (messenger ribonucleic acid).
Pfizer COVID-19 Vaccine Side Effects
During clinical trials for the Pfizer COVID-19 vaccine, these were some of the common side effects:
- Pain and swelling on the arm where the shot was given
- Fever
- Chills
- Fatigue
- Headache
More people felt the side effects after the second dose of the vaccine.
Moderna COVID-19 Vaccine, Also Known As spikevax™, for Everyone 6 Months and Older
The Moderna COVID-19 vaccine, called spikevax™, is an mRNA vaccine. It is one of the mRNA vaccines recommended for anyone ages 6 months and older. The CDC’s recommended vaccine schedule is below.
If you or your child are moderately-to-severely immunocompromised, you will have a different vaccine schedule. This includes children and adults on high doses of corticosteroids (like prednisone), who have received an organ transplant, or have other serious health conditions.
Children 6 months to age 17 years
- Primary doses: Two doses four to eight weeks apart
- Booster doses: Not recommended at this time
- Immunocompromised:
- Three primary doses (first two doses four weeks apart and the third at least four weeks after the second dose)
- Three primary doses (first two doses four weeks apart and the third at least four weeks after the second dose)
People ages 18 and older
- Primary doses: Two doses four to eight weeks apart
- Booster doses: At least five months after the second dose
- Immunocompromised:
- Three primary doses (first two doses four weeks apart and the third at least four weeks after the second dose)
- One booster (at least three months after the third primary dose)
People ages 50 and older should get a second mRNA booster at least four months after the first booster.
If you got the Moderna vaccine for your first shot, the CDC recommends that you get the Moderna shot for your additional primary shots.
Children 5 to 11 years of age will receive a lower dose of the vaccine than people 12 and older. If you have any questions about the vaccine for your child, talk with your family doctor or pediatrician.
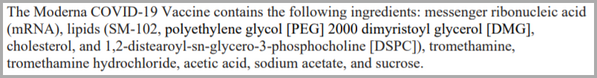
Moderna COVID-19 Vaccine Ingredients
The Moderna vaccine does not contain any food proteins, latex, or preservatives. It does contain mRNA (messenger ribonucleic acid).
Moderna COVID-19 Vaccine Side Effects
During clinical trials for the Moderna COVID-19 vaccine, these were some of the common side effects:
- Pain and swelling on the arm where the shot was given
- Fever
- Chills
- Fatigue
- Headache
- Muscle pain
- Joint pain
- Swollen lymph nodes in the same arm where the injection was given
- Nausea
- Vomiting
More people felt the side effects after the second dose of the vaccine.
Novavax, COVID-19 Vaccine, for People Ages 18 and Older
On July 13, 2022, the Food and Drug Administration (FDA) authorized the Novavax COVID-19 vaccines for emergency use. The CDC also recommends Novavax as an option for people ages 18 and older.
Novavax is given in two primary doses three to eight weeks apart. If you are moderately-to-severely immunocompromised, two doses are given three weeks apart. Novavax boosters are not authorized at this time.
Novavax is an adjuvanted vaccine. This vaccine is similar to the traditional flu vaccines that have been given for many years.
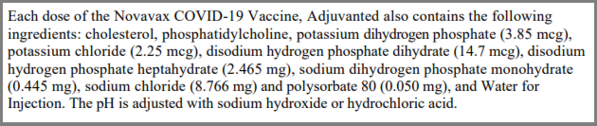
Novavax COVID-19 Vaccine Ingredients
Novavax does not contain any food proteins, latex, or preservatives.
Novavax COVID-19 Vaccine Side Effects
During clinical trials for the Novavax COVID-19 vaccine, these were some of the common side effects:
- Pain, redness, and swelling on the arm where the shot was given
- Fever
- Nausea/vomiting
- Muscle aches/joint pain
- Fatigue
- Headache
Johnson & Johnson (Janssen) COVID-19 Vaccine for People Ages 18 and Older in Certain Situations
The J&J vaccine is a viral vector vaccine given in one shot. It is available for people 18 and older.
According to the CDC, the Pfizer and Moderna COVID-19 vaccines are preferred over the J&J vaccine, due to the risk for severe side effects. But you may consider the J&J vaccine in the following situations:
- You’ve had a severe reaction after having an mRNA vaccine
- You are allergic to an ingredient in the Pfizer and Moderna vaccines
- You do not have access to the Pfizer or Moderna vaccines
- Despite safety concerns, you prefer to get the J&J vaccine
Here is the vaccine schedule for the J&J vaccine:
- Primary dose: One shot
- Booster doses: One booster at least two months after the primary dose for people under age 50; people 50 or older should get an mRNA dose at least four months after the second dose
- Immunocompromised:
- One primary dose
- Three boosters
- First booster: Four weeks after the primary shot (mRNA is preferred, but you may consider the J&J shot in some situations)
- Second booster: At least two months after the first booster (if you get an mRNA shot for your first booster, you cannot get the J&J shot for your second booster)
- Third booster: At least four months after the second booster
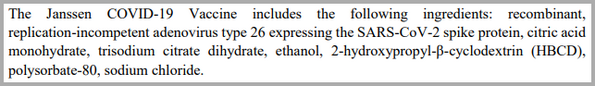
Johnson & Johnson COVID-19 Vaccine Ingredients
The J&J vaccine does not contain any food proteins, latex, or preservatives.
Johnson & Johnson COVID-19 Vaccine Side Effects
During clinical trials for the J&J COVID-19 vaccine, these were some of the common side effects:
- Pain, redness, and swelling on the arm where the shot was given
- Fever
- Nausea
- Muscle aches
- Fatigue
- Headache
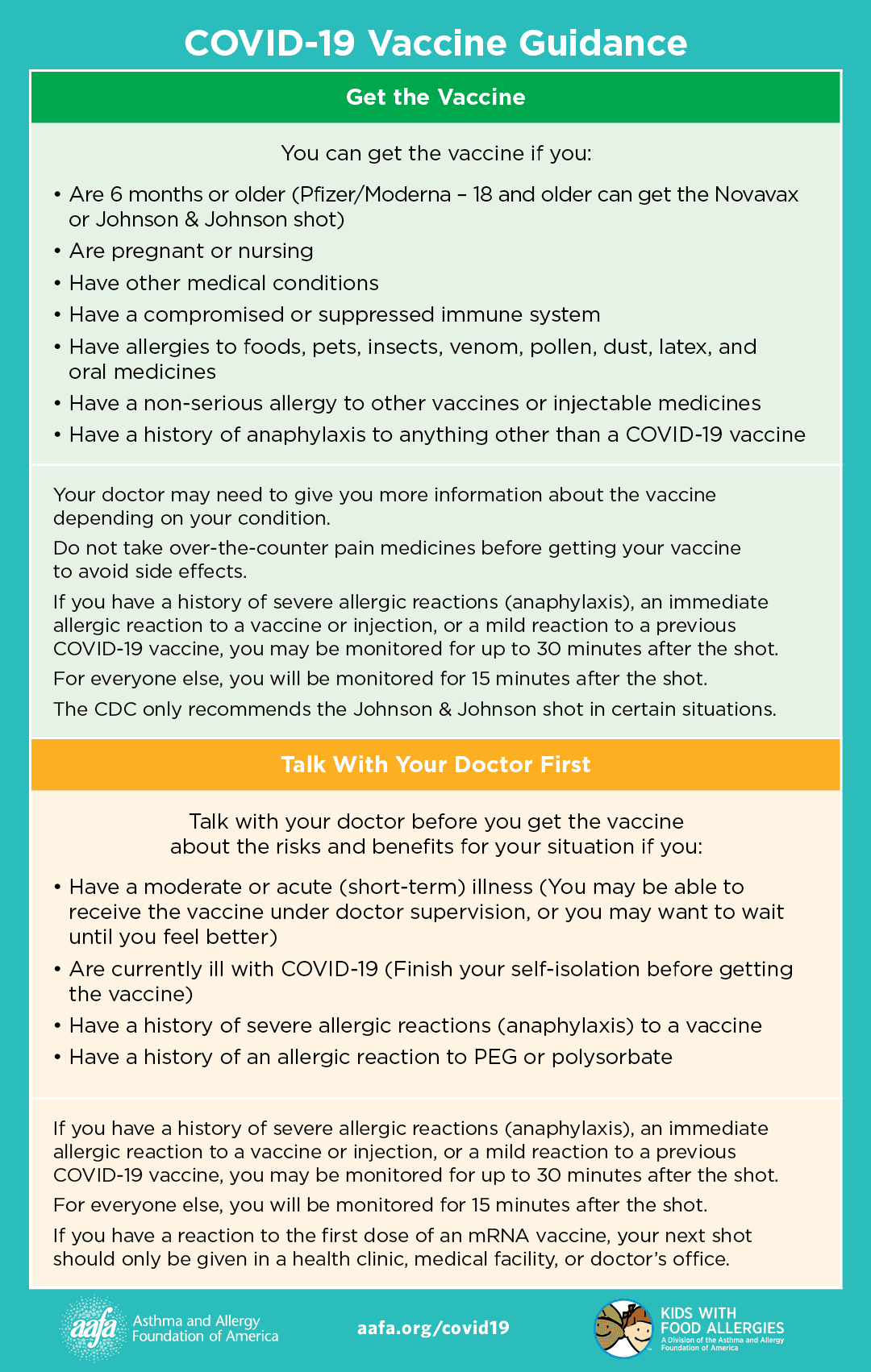
Who Can Get a COVID-19 Vaccine?
The COVID-19 vaccine is free to everyone. You can get your shot at a local pharmacy, clinic, or vaccination center. Go to vaccines.gov to find a location.
You can get a COVID-19 vaccine if you:
- Are ages 6 months and older
- Have a medical condition
- Are immunocompromised or immunosuppressed
- Are pregnant and lactating (nursing)
- Have allergies to food, pets, insects, venom, pollen, dust, latex, and oral medicines
- Have a non-serious allergy to other vaccines or injectable medicines
- Have a family history of anaphylaxis or any other history of anaphylaxis to anything other than a vaccine or injectable medicine
Your doctor may need to give you more information about the vaccine depending on your condition.
If you have a history of severe allergic reactions (anaphylaxis), an immediate allergic reaction to a vaccine or injection, or a mild reaction to a previous COVID-19 vaccine, you may be monitored for up to 30 minutes after the shot.
Talk with your doctor about risks and benefits before getting a COVID-19 vaccine and get the shots in a clinic or doctor’s office if you have a:
- Moderate or acute (short-term) illness (such as the flu)
- History of anaphylaxis to another vaccine or injectable medicines
- Severe or immediate allergic reaction to previous dose or any ingredient (also called “excipients” or “components”) of a COVID-19 vaccine
- History of an allergic reaction to PEG or polysorbate
Many people who have a history of PEG or polysorbate allergy have been successfully vaccinated for COVID-19.
If you are allergic to polysorbate, you should not get the J&J vaccine.
If you have a reaction to the first dose of an mRNA vaccine, your next shot should only be given in a health clinic, medical facility, or doctor’s office.
People who currently have or recently had COVID-19 should finish isolation and talk to their doctors about when to get the vaccine. You may want to wait until three months to get your next dose after your COVID-19 symptoms started. This also applies if you received COVID-19 monoclonal antibody treatment or convalescent plasma while you had COVID-19. You should get vaccinated and boosted even if you have had COVID-19 in the past.
What Are the Recommendations for COVID-19 Vaccines for Pregnant People?
If you are pregnant or are thinking of becoming pregnant, you should get the COVID-19 vaccine. Pregnant people are at a higher risk for severe COVID-19 when compared to non-pregnant people.1 If you had a recent pregnancy (for at least 42 days following the end of pregnancy), it may also raise your risk for developing severe COVID-19. If you get COVID-19 while pregnant, you are at increased risk for preterm birth (delivering the baby earlier than 37 weeks) and other poor pregnancy outcomes.2
What Do I Need to Know Before I Get My COVID-19 Vaccine?
If you have a history of severe allergic reactions (anaphylaxis), an immediate allergic reaction to a vaccine or injection, or a mild reaction to a previous COVID-19 vaccine, you may be monitored for up to 30 minutes after the shot.
Do not take over-the-counter pain medicines like acetaminophen (Tylenol) or ibuprofen (Advil) before getting a COVID-19 vaccine to reduce side effects if you don’t take these medicines regularly. Taking over-the-counter pain medicines or anti-inflammatories may stop the vaccine from working as it should and reduce its ability to make antibodies. Talk with your doctor about taking pain medicines after you get the shot.
You can get the flu shot and the COVID-19 vaccine at the same time.
If you get allergy shots (immunotherapy) or biologic shots or infusions, talk with your allergist if your shot schedule overlaps with getting the COVID-19 vaccine. There is not a lot of data on allergy shots, biologics, and the COVID-19 vaccine at this time. But to help reduce confusion if you have local reactions or side effects, it may help to spread these out by a few days.
What Do I Do If You Have Side Effects to the COVID-19 Vaccine?
The CDC is asking people to help report any side effects to the COVID-19 vaccines. V-safe is a smartphone-based tool that uses text messaging and web surveys to provide personalized health check-ins after you receive a COVID-19 vaccination. Through v-safe, you can quickly tell the CDC if you have any side effects after getting the COVID-19 vaccine. Depending on your answers, someone from the CDC may call to check on you and get more information. And v-safe will remind you to get your second COVID-19 vaccine dose if you need one. The information on how to register for v-safe can be found on the vaccination record card you receive when you get the shot. If you cannot find your card, please contact your health care provider.
What Activities Can I Do Safely If I Am Fully Vaccinated and Boosted Against COVID-19? Do I Have to Wear a Mask?
Once you are fully vaccinated and boosted, you can go back to doing many of the activities you did before the pandemic. But it’s a good idea to wear a mask in public indoor places, even if you are fully vaccinated and boosted.
Continuing to wear a face mask may have benefits. If you have asthma or allergies, masks can help protect you from pollen and other allergens and irritants that trigger symptoms. Masks also can protect you from respiratory infections like the flu, COVID-19, and even the common cold. Masks provide increased protection for people who are immunocompromised.
Universal indoor masking is recommended for all teachers, staff, students (ages 2 and older), and visitors to schools, regardless of vaccination.
If you have a condition or are taking medicines that weaken your immune system, talk with your doctor about which activities are safe to do.
Consider postponing unnecessary travel.
What Should I Do If I’m Not Fully Vaccinated and/or Boosted Against COVID-19?
If you have not received a COVID-19 shot yet, plan to get vaccinated as soon as possible. If you have received your primary series of the COVID-19 vaccine but have not gotten a booster shot, plan to do so as soon as possible.
People who are unvaccinated and not boosted are at the higher risk of getting COVID-19, spreading it to other people, and becoming hospitalized and/or dying of the virus. If you believe you are not eligible for the vaccine due to your medical conditions, talk with your doctor to see what options may be available to you.
Are Vaccines Effective Against COVID-19 Variants?
Although you may still get COVID after being fully vaccinated, vaccines can help prevent severe symptoms and complications, such as death. You will likely experience mild symptoms compared to someone who is not vaccinated. Vaccines provide at least some protection against new variants, such as the Omicron strains.
In order to prevent new variants, stopping the spread of COVID-19 is important. We encourage you to wash your hands frequently, wear a mask, practice physical distancing, and avoid crowded areas.
Medical Review July 2022 by Mitchell Grayson, MD
JOIN NOW
References
1. Zambrano LD, Ellington S, Strid P, et al. Update: Characteristics of Symptomatic Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status — United States, January 22–October 3, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1641–1647. DOI: http://dx.doi.org/10.15585/mmwr.mm6944e3
2. Allotey J, Stallings E, Bonet M, Yap M, Chatterjee S, Kew T et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis BMJ 2020; 370 :m3320 doi:10.1136/bmj.m3320


Comments (3)