Update – July 25, 2021
We updated this blog post to include updated information and guidance from the Asthma and Allergy Foundation of America (AAFA) and the Centers for Disease Control and Prevention (CDC).
Note: Because this is a constantly changing situation, any data in this blog post may not represent the most up-to-date information. We will update this blog when possible.
In December 2019, a new coronavirus named SARS-CoV-2 started spreading and triggered a pandemic (worldwide outbreak). This coronavirus causes an illness known as COVID-19.
The coronavirus spreads through close contact from person to person. A person with the virus can spread it to others by talking, coughing, sneezing, singing, or breathing. The virus will be in large or small droplets that are exhaled from the mouth or nose out into the air.
If you are within 6 feet (2 meters) of someone who is ill with COVID-19, you may be at greatest risk for becoming infected. But it may be possible to catch the virus even if you are more than 6 feet away from an infected person because very small droplets can spread in the air. If someone who is sick coughs on or near your face, you may get infected. People may be infected with the coronavirus and not show any symptoms. They may spread the virus without knowing it. The virus may also spread through direct contact with a person who has COVID-19.
What Are the Symptoms of COVID-19?
According to the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO), COVID-19 symptoms can include:
- Fever
- Chills
- Cough
- Shortness of breath or trouble breathing
- Feeling tired and weak
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Stuffy or runny nose
- Nausea or vomiting
- Diarrhea
If you or someone you know has these emergency warning signs, call 911 or go to the emergency room immediately:
- Trouble breathing or shortness of breath
- Pain or pressure in the chest that doesn’t go away
- Newly confused
- Can’t wake up or stay awake
- Cyanosis which is tissue color changes on mucus membranes (like tongue, lips, and around the eyes) and fingertips or nail beds – the color appears grayish or whitish on darker skin tones and bluish on lighter skin tones
According to the CDC, this list may not include all symptoms. If you have any symptoms that are severe or concerning, call your doctor.
The CDC warns that symptoms may appear two to 14 days after coming in contact with the virus.
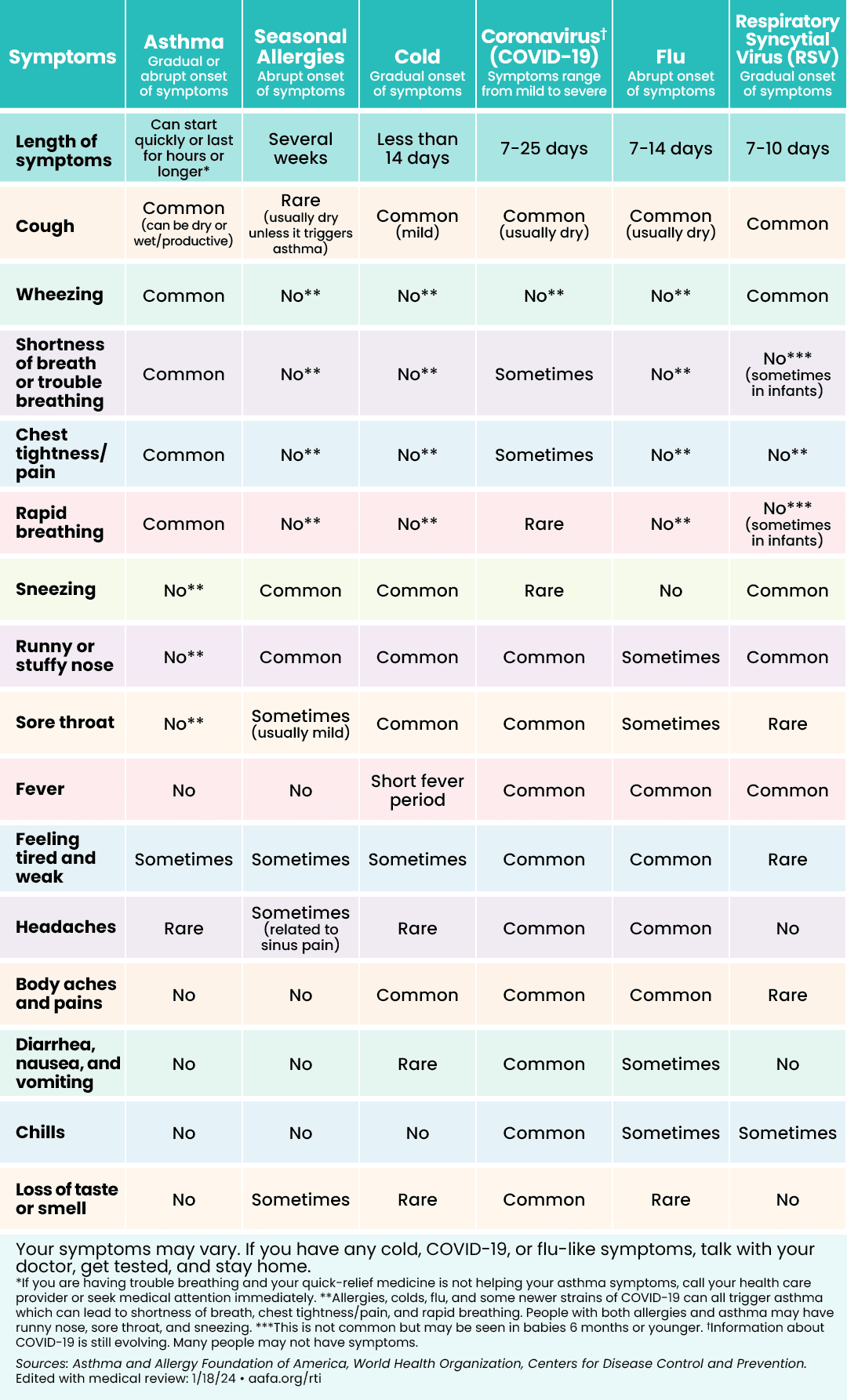
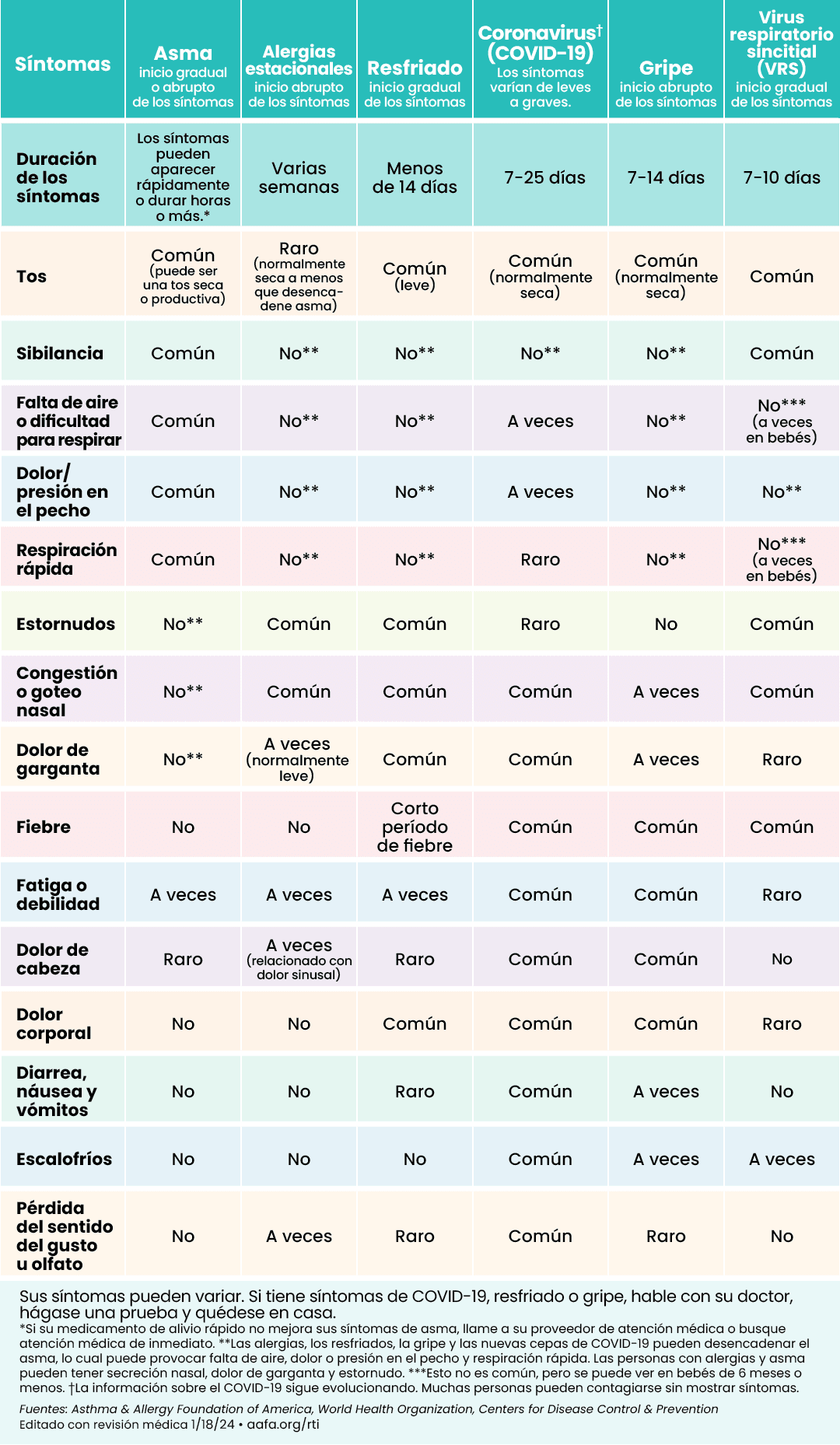
How Can I Tell the Difference Between Asthma, COVID-19, the Flu, a Cold, or Seasonal Allergies?
Some symptoms are similar between these respiratory illnesses. Respiratory illnesses may worsen asthma, so it’s important to keep taking your asthma medicines. If you have a fever and a cough, call your doctor. If you have seasonal allergies, there are things you can do to treat them at home. If your allergy symptoms are hard to control, make an appointment with an allergist.
This chart can help you figure out if you may be feeling symptoms of asthma, allergies, or a respiratory illness like COVID-19, the flu, or a cold:
Are People With Asthma at Risk of Severe Illness From COVID-19?
Many studies show that having asthma does not put you at a greater risk of getting COVID-19 or having severe COVID-19.1,2,3 A study published in “The Journal of Allergy and Clinical Immunology: In Practice” (JACI: In Practice) found that people with well-controlled asthma have less severe COVID-19 outcomes than people with uncontrolled asthma.4
The CDC continues to list moderate-to-severe asthma as a chronic lung disease that can make you more likely to have severe illness from COVID-19.
No matter what, it is important to keep your asthma well-controlled. If your asthma is not under control, you are at a greater risk in general of having an asthma episode or attack, going to the emergency room, staying in the hospital, or even death. If you feel like your asthma is not well-controlled, talk with your doctor as soon as possible.
Even though people with asthma are not at the highest risk for COVID-19, it is still important to keep your asthma under control. Common medicines you may take for asthma and allergies do not increase your risk of getting COVID-19. They will help you keep your asthma under control. You are at greater risk for having an asthma attack if you stop taking your medicines. Take your medicines at the first sign of symptoms as listed on your asthma action plan. Continue to take these medicines as prescribed:
- Quick-relief medicine (such as albuterol)
- Inhaled corticosteroids (controller medicines)
- Oral corticosteroids (such as prednisone)
- Biologics
- Antihistamines (allergy medicine)
- Proton pump inhibitors for acid reflux
- Nasal allergy sprays
- Allergy shots
If you have any questions about asthma medicines and COVID-19, talk with your doctor.
If you need to take quick-relief medicine (such as albuterol) for an asthma episode, use an inhaler (with a spacer if directed by your doctor) if possible. Using a nebulizer can increase the risk of sending virus particles in the air if you are sick. But if you have a nebulizer and solution, it is OK to use it to treat an asthma episode. When using a nebulizer, limit the number of people in the room or use it in a room by yourself.
How Can I Avoid Getting COVID-19 (And Other Respiratory Infections)?
The following steps will help you avoid COVID-19, the flu, and other respiratory infections:
1. Get your vaccines.
Vaccines can help protect you, your loved ones, older adults near you, teachers, and essential workers from getting a respiratory infection. They can also cut down your symptom severity if you do get sick. Vaccines reduce the burden on our health care system by reducing the number of people who get COVID-19 or the flu.
Everyone who is 6 months and older can get a COVID-19 vaccine for free with no out-of-pocket costs in the United States. There are currently four vaccines available: Pfizer, Moderna, Johnson & Johnson (J&J), and Novavax.
Visit vaccines.gov to find out where you can get the COVID-19 vaccine near you. Most people can get the COVID-19 vaccine with no issues. Allergic and adverse reactions are rare.
The flu vaccine is recommended for everyone age 6 months and older with rare exceptions.
It is safe to get both the COVID-19 vaccine and the flu vaccine at the same time.
2. Wear a mask.
Face masks can help reduce the spread of the coronavirus. They can benefit people who are vaccinated and unvaccinated alike. Some people may have COVID-19 and not show symptoms for a few days, while some may not have any symptoms at all. And some vaccinated people have gotten breakthrough infections, which have usually been mild.
Wear a mask that fits snugly on your face, and covers your nose, mouth, and beard completely. Wear a mask when you leave your home, if you are caring for someone at home who is sick, and if you have been exposed to someone with COVID-19. People with asthma should be able to wear face masks.
Face masks offer other benefits as well. They can reduce your exposure to pollen, air pollution, and other respiratory infections like the flu.
3. Keep a physical distance from people outside your household.
In general, the more closely you interact with other people and the longer that interaction, the higher the risk of coronavirus or flu spread. Try to stay home when possible when these illnesses are spreading in your community. Avoid large crowds of people, especially in indoor locations. When in public, keep at least 6 feet apart. Stay away from people who are sick or have been in contact with someone who is sick. Even when you’re at home with family, don’t share makeup, food, dishes, or eating utensils.
Postpone any unnecessary travel during the COVID-19 pandemic. See the CDC’s guidelines on how to protect yourself at specific locations and in certain situations, such as shops, public places, gatherings, and more.
4. Wash your hands properly and often.
Use soap and warm water to wash your hands for 20 to 30 seconds. Always wash your hands before and after eating and after coughing or sneezing. Don’t touch your eyes, nose, or mouth.
If you don’t have access to running water, use an alcohol-based hand sanitizer that is at least 60% ethyl alcohol (ethanol) or 70% isopropyl alcohol (isopropanol).
5. Make sure your indoor spaces are well-ventilated and have good indoor air quality.
If you are staying indoors more because of COVID-19, be mindful of the quality of your indoor air. The air inside our homes can often be more polluted than the air outside. Unhealthy indoor air can be full of asthma triggers and allergens that can cause symptoms and make your asthma harder to control. Take steps to improve and maintain healthy indoor air quality.
Air circulation is important too. Keep your indoor spaces well-ventilated by opening windows or doors, using fans, running air cleaners, or using proper air filters in your HVAC system.
Current evidence shows the risk of the coronavirus spreading is much lower outdoors than indoors. Good ventilation in your indoor environment may help reduce the spread of the coronavirus. It may also affect the risk of transmission (how fast it spreads).
On days when pollen is low and air quality is good, open your windows to let in fresh air. Run your HVAC system as much as possible (especially when windows are closed). Use high efficiency air filters in your HVAC system and replace them at least every three months.
6. Take care of your health.
Take your asthma control medicines as directed to keep your airways open. Eat well and get enough sleep.
Pollen (such as grass or ragweed pollen) may impact people across the U.S. too. Seasonal allergies can affect people with allergic asthma. If pollen allergies trigger asthma symptoms for you, be sure to follow your allergy treatment plan to keep your allergies under control to prevent asthma episodes or attacks.
If you stopped seeing your allergist or getting allergy shots (immunotherapy) during the COVID-19 pandemic, consider making an appointment soon. Keeping up with your regular allergist visits is an important part of keeping your asthma controlled.
The most important thing you can do is to keep your asthma under control. If your asthma is not under control, call your doctor right away.
In general, tracking your symptoms and following your asthma action plan are key to managing your asthma. Some people use peak flow meters to monitor their airways. Monitoring your blood oxygen levels with a pulse oximeter (or “pulse ox”) is not a recommended part of home management of asthma. Many pulse oximeters you can buy for home use are not as accurate as medical grade devices.
It is important to remember that the symptoms you feel should always come before pulse ox and peak flow numbers. But if your peak flow numbers are down and you don’t have symptoms, follow your asthma action plan and contact your doctor.
There are no data demonstrating that monitoring your pulse ox through an oximeter or smartphone app will help manage your asthma. As always, talk with your doctor about the best ways to monitor your symptoms and asthma control.6
If I Think I Have COVID-19, What Should I Do?
If you start having symptoms of COVID-19, get tested or take an at-home test. If you have mild symptoms and are not at high risk for having more severe COVID-19, you do not need to call your doctor. Call your local health department within 24 hours to let them know so they accurately report local cases.
If you are at high risk for severe COVID-19, call your doctor within 24 hours if you test positive. They may want to you to take the medicine Paxlovid.
Many pharmacies have various testing options (including at-home or drive-thru tests). The United States Postal Services is providing free at-home COVID-19 tests. U.S. households can get eight rapid antigen COVID-19 tests for free. To receive them, you’ll need to complete an online form. Please note: You will not need to enter any credit or debit card details to place the order.
Some doctors may offer telehealth (video or virtual appointments). If that is an option, ask your insurance company if telehealth is covered under your plan. And if you have Medicare, you might be able to have a virtual visit with your doctor. The government expanded the coverage of telehealth services during the COVID-19 pandemic.
Stay home and isolate from family members so you don’t spread the coronavirus to other people.
Medical Review, July 2022 by Mitchell Grayson, MD
JOIN NOW
References
1. Chhiba, K.D., Patel, G.B., Vu, T.H.T, Chen, M.M., Guo, A., Kudlaty, E., Mai, Q., Yeh, C., Muhammad, L.N., Harris, K.E., Bochner, B.S., Grammar, L.C., Greenberger, P.A., Kalhan, R., Kuang, F.L., Saltoun, C.A., Schleimer, R.P., Stevens, W.W., & Peters, A.T. (2020). Prevalence and characterization of asthma in hospitalized and non-hospitalized patients with COVID-19, Journal of Allergy and Clinical Immunology. https://doi.org/10.1016/j.jaci.2020.06.010.
2. Butler, M. W., O’Reilly, A., Dunican, E. M., Mallon, P., Feeney, E. R., Keane, M. P., & McCarthy, C. (2020). Prevalence of comorbid asthma in COVID-19 patients. Journal of Allergy and Clinical Immunology. https://doi.org/10.1016/j.jaci.2020.04.061
3. Lieberman-Cribbin, W., Rapp, J., Alpert, N., Tuminello, S., & Taioli, E. (2020). The Impact of Asthma on Mortality in Patients With COVID-19. Chest. https://doi.org/10.1016/j.chest.2020.0air pol.575
4. Huang, B. Z., Chen, Z., Sidell, M. A., Eckel, S. P., Martinez, M. P., Lurmann, F., Thomas, D. C., Gilliland, F. D., & Xiang, A. H. (2021). Asthma disease Status, COPD, and COVID-19 severity in a large Multiethnic POPULATION. The Journal of Allergy and Clinical Immunology: In Practice. https://doi.org/10.1016/j.jaip.2021.07.030
5. Kampf, G., Todt, D., Pfaender, S., & Steinmann, E. (2020). Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. Journal of Hospital Infection, 104(3), 246–251. doi: 10.1016/j.jhin.2020.01.022
6. Heneghan, C. (2018, January 30). Self-management of asthma – is there an app or pulse oximeter for that? Retrieved from https://blogs.bmj.com/bmjebmsp...-app-pulse-oximeter/

Comments (131)